Update from the ENT team, they came in and used a scope to take measurements so that they can order him a custom trach. He said they do still want to watch him carefully in ICU until later in the week. He likely then will move to another room here in the hospital with plans for another surgery next week to replace his trach with a better fitting one. Didn't think our visit was going to be this long or have this many surgeries, but getting a good solid airway will help us to begin tackling the initial issue.
I think our favorite team is the Physical Therapy team. The person helping yesterday and today was Jennifer Underdown. She's very caring and compassionate and is Chris's biggest cheerleader (besides me course). Today she helped him get up and take a short walk out into the hallway, then after a bit of rest another longer walk in the hallway. Then later got Chris situated in a comfortable chair and took us on a circular tour of the surgical and cardiac ICU. She told him that there was a toll and that he had to high five or fist bump people as she pushed him by. It was amazing how familiar many of these faces have become as many of them have been in his room at sometime or another.
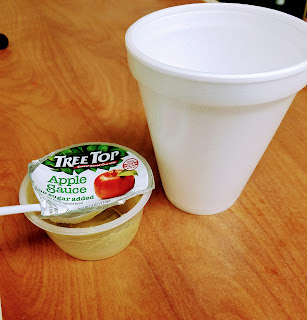 Another positive step today was meeting with a speech therapist. He's been on a feeding tube since later last week and meeting with her today started the process to be able eat again. She went slowly and first started with an ice cube. Can you imagine how amazing that felt in his mouth after being intubated! Then sips of water, then applesauce,
Another positive step today was meeting with a speech therapist. He's been on a feeding tube since later last week and meeting with her today started the process to be able eat again. She went slowly and first started with an ice cube. Can you imagine how amazing that felt in his mouth after being intubated! Then sips of water, then applesauce,
then finally a saltine cracker. Good news is that he was able to taste. :) After she was done testing we asked if he could finish what was left of the apple sauce or water. He quickly (but carefully) gobbled it up. They have to pass the findings along to the ENT team before they will allow him to make a decision on diet. Hopefully soon he'll be able to at least start drinking or eating soft foods. He loves the chocolate pudding here, and we hear they have ice cream too, so we're crossing our fingers that they will give the OK tonight before they leave.
She also gave us more information about learning how to speak again. At this point the trach is taking up most of the space in his airway and there isn't enough extra room for the air to move around. This is what is needed to make your vocal cords work. After they replace the trach next week with a new one, as long as there is enough space for air to flow they can fit him with a different valve that will allow him to speak. At this point because the speaking valve closes off the airway, he wouldn't be able to breath with that adapter. Being able to sit up for most of the day so far, he's great at communicating with a pad of paper and pen. It will be great to hear him speak again.
It's amazing to me the number of staff here at the hospital that are watching out for us. Talked again to social work as well as our case manager who both are working to make sure that everything is in place for Chris to eventually transition back to home. Also have been working with one of the people in charge on the floor here to make getting back home as easy as possible. They are thinking that instead of a regular room, they might instead move him to in-patient rehab where much of his time will be filled with different therapies and classes (for both of us) to learn all about this new life with a trach.
I am so glad that Chris has been able to eat something. That is where my dad ran into problems after his breathing tube was removed. Keep up the great work Chris!!
ReplyDelete