For our season, it's a time to wait and learn patience. Just over three months ago we were on the tail end of a very long hospital stay. While here then, the season's changed from spring to summer (typical of unpredictable Utah weather a little bit of snow in between). Now, here we are again at the University of Utah hospital for another surgery. On the way here there were many signs of the change of seasons, it's still hot outside, but it's back to school time which means fall will be here shortly. There was a traffic sign as we neared the "U" warning us... "Watch for incoming freshman".
It's just after 1:00 in the afternoon and Chris was taken back about an hour ago. Today's surgery is the same as the first one in May, a dilation to open up his airway. When we scheduled this one, the prime goal was to remove the trach. Talking with the doctor today, I'm not so sure that this will happen. If anything, they might change it for a different one.
Compared to the past two surgeries, this time the waiting room is bustling with activity. People constantly coming and going, phones ringing, people receiving updates, nurses walking around with stacks of binders (aka charts), even a lady with a service dog for people to pet if it will help calm their nerves.
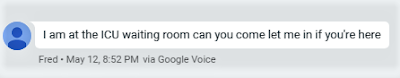
His first surgery in May was the complete opposite. Late at night with no one manning the information desk, and not a soul in the waiting room but me. A situation that in other situation would have terrified me, ended up being precisely what I needed. Through previous trials I had been prepared me for it and given the strength and comfort to endure. I was able to take solace in the quiet moment by writing in my journal. When I was able to see him in recovery, and things went downhill I was able to focus completely on being with him in the moment.
His second surgery that stay, when they added the trach, was similar. It was on Mother's Day Sunday, and this time I surrounded by family, but we had the entire waiting room to ourselves. Together we waited and some very tender moments followed when everyone was reunited in the SICU.
Today I am alone, but I'm fine. I know I could have asked someone to be with me, but today should be a simple procedure and I'm at peace. When I was searching for the picture of the tree above, this one also came up in my search. It fit my feelings also, we've both faced some scary things but is our faith that has given us courage. In the event we end up in the ICU again, it's not the terrifying place it once was, the nurses and doctors there are amazing.
_______________________________________________________________________________
Surgery today was longer than they predicted. Got an update from Dr Smith about 3:00. From the pictures he showed it looks like the stenosis has returned. It didn't look as bad as in May, but it didn't look as open as the last office visit. They had to use the balloon multiple times to stretch it. Chris was having a tough time coming out of anesthesia and that he wanted him observed in recovery to determine if he should be taken to ICU.


He didn't feel it would be wise to remove his trach completely, so instead he changed it out for a different kind. They replaced the custom one....with a tube so long that it reaches to the bottom of his trachea. with something different. What he had before is somewhat similar to the one to the left but with a much longer tube. The one they put in today is like the one on the right. It sticks into his throat and and is held in place on the inside with flanges. While not the complete removal of the trach we were hoping for, we know it's a step in a better direction.
About a half an hour after the update from Dr Smith, they let me go back to see him. He had stabilized enough that they allowed me to sit with him. He stayed stable the entire hour and a half I was there. He was tired and in and out, but when he saw me he gave me a great big smile (he sure knows how to make a gals day). Once they finally had a room free they moved us to a regular room on the Acute Neuro floor. Took some time to get situated and bring in everything he needed, but he's all settled in. He was able to eat dinner, and said his throat is super sore, but otherwise he is doing well. Dr Smith said that cold things should help with that, I see lots of ice cream in his future.
Overall a long day, but very grateful for all the prayers said on our behalf today.
This year has by far been the most challenging "seasons" of my life, and I'm sure that Chris would agree it has also been his. We've been tempered in the refiner's fire and it's changed both of us in many ways, but one of its purposes has been to make us stronger. Hopefully that strength won't be for more trials yet ahead, but our journey is not yet over.